Piriformis syndrome is a neuromuscular condition that occurs when the piriformis muscle, located deep in the buttock, compresses or irritates the sciatic nerve. This can lead to pain, numbness, and tingling along the back of the leg and into the foot, causing the symptoms of sciatica. This is, indeed, a form of sciatica. But understanding the cause of the symptoms is key for effective treatment, so your osteopath may give you the more specific diagnosis of “piriformis syndrome”.
Understanding Piriformis Syndrome
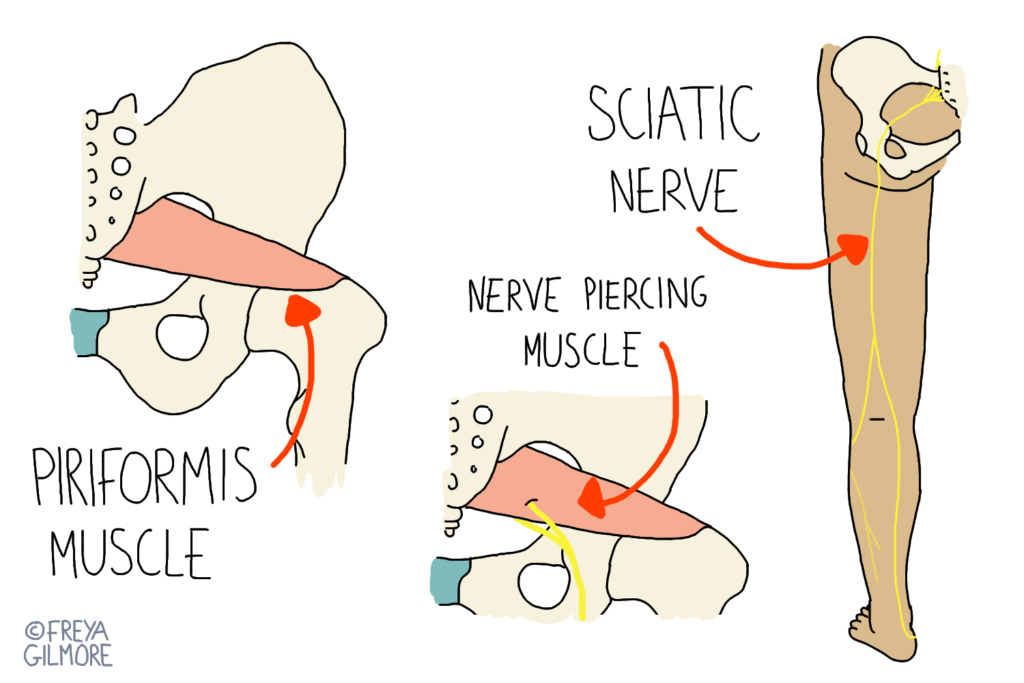
The piriformis muscle is a small, flat muscle found deep in the buttock. It stretches from the base of the spine, to the top of the thigh bone. Its roles are to stabilise the hip and turn the thigh outward. The sciatic nerve, the longest and largest nerve in the body, forms in the lower back and travels through the buttock, down the back of the leg, and into the foot.
In most people, the sciatic nerve passes underneath the piriformis muscle. However, just like we don’t all look the same on the outside, there is wide variation in our internal anatomy too. For some people, the sciatic nerve passes through or over the muscle. When the muscle becomes tight or inflamed, it can press on the nerve, causing the characteristic symptoms of sciatica. This variation in the relationship between the muscle and the nerve may make some people more susceptible to developing the condition.
Risk Factors and Affected Demographics
Several factors can increase the risk of developing piriformis syndrome. Repetitive activities that involve prolonged sitting or movements that excessively engage the piriformis muscle can lead to overuse and tightness. For example, athletes who participate in running, cycling, or activities that involve frequent changes in direction are at a higher risk of developing piriformis syndrome. Prolonged sitting, particularly with poor posture, can also contribute to muscle tightness and irritation of the sciatic nerve. In either case, a sudden change in routine, such as needing to spend more time at the desk, or increasing/starting training can both impact the muscle and lead to symptom development.
In addition to lifestyle factors, certain anatomical and biomechanical variations may predispose individuals to piriformis syndrome. Such as:
- leg length discrepancies or scoliosis
- sacroiliac joint dysfunction
- abnormal foot mechanics
These factors may put increased stress on the piriformis muscle, making the individual more susceptible to the condition. However, the body is a brilliant adaptor, so the presence of these factors are by no means a guarantee that the symptoms will develop. Piriformis syndrome can affect individuals of any age, but it is more commonly seen in adults, particularly those between the ages of 30 and 50. Women are more likely to be affected than men at a ratio of 6:1. One reason for this imbalance may be the demands of pregnancy on the lower back: sciatica is a common complaint in pregnancy.
Osteopathy and Piriformis Syndrome
Osteopathy offers an effective approach to managing piriformis syndrome by addressing the underlying muscle tightness and nerve irritation. We use hands-on techniques to relieve pain, improve mobility, and restore balance to the affected areas. Soft tissue work is a key component of osteopathic treatment for piriformis syndrome. We also use gentle massage and stretching techniques to release tension in the piriformis muscle, reducing pressure on the sciatic nerve. This helps alleviate pain and improve the range of motion in the hip joint. Finally, joint mobilisation techniques aim to address any underlying biomechanical issues that could be contributing to the condition.
When nerve symptoms are involved, desensitising techniques can be an important aspect of treatment. If the sciatic nerve is particularly over-excited, gentle techniques can help reduce nerve sensitivity and alleviate the associated symptoms of pain, numbness, and tingling. This can be as simple as gentle massage over the symptomatic area of the leg to help wind down the nervous system’s response to irritation. In addition to work in the treatment room, we typically incorporate home exercises and stretches into our treatment plans. These exercises have the dual benefit of helping to maintain flexibility and strength in the affected area. By keeping the area strong, we aim to prevent or minimise future episodes of piriformis syndrome.
Click here to make an appointment with Beverley for your piriformis syndrome
